_edited.jpg)
Christina's Graduation with Leadership Distinction in Research e-portfolio
Access to mental health care among the Latinx population in South Carolina
Problem Statement
scroll
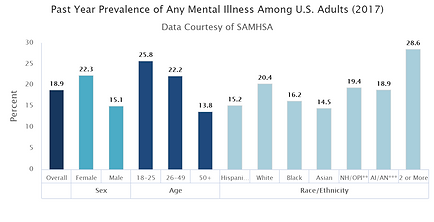
Mental health is a state of emotional and psychological well-being that is essential for determining the way we handle stress, act in social situations, and make decisions. Anxiety, phobia, major-depressive, substance abuse, and impulse control disorders are some of the most prevalent psychiatric disorders in the United States (Kessler, Chiu, Delmer, & Walters, 2005). According to the National Institute of Mental Health (NIMH), an estimated 18.9% of all United States adults had some mental illness in 2017. Globally, an estimated 1 billion people (1 in 7) are affected by mental and substance abuse disorders (Ritchie, 2018). However, in 2001 66% of countries allocated 1% or less of their total health budgets to mental health (World Health Organization, 2001).
Latino/Hispanic Communities And Mental Health
Read More >
Data from The National Latino and Asian American Study (NLAAS) showed an overall prevalence of psychiatric disorders across Latino subgroups (Mexican, Puerto Rican, Cuban and Other) in men to be 28.1% and 30.2% in females (Alegría et al., 2007). Only 32% of Latinos with psychiatric needs sought service (Lee, Laiewski, & Choi, 2014). Cost, lack-of insurance, and language proficiency are all factors that impede service utilization (Bridges et al., 2012; Lee, Laiewski, Choi, 2014). Unfortunately, this has led Latinx Americans to be more likely to reach inpatient care for mental disorders through emergency services, and significantly less likely to self-refer (Delphin-Rittmon et al., 2015).
In South Carolina, anxiety, depression, and substance use disorders are some of the most prevalent mental health disorders amongst Whites, Blacks, and Hispanics. Interestingly, South Carolina, the Latinx population received significantly fewer mental health diagnoses in proportion to their population than White and Black counterparts (Lorenzo-Blanco et al., 2016). Conversely, the Latinx population in South Carolina had over three times the diagnoses for acute reaction to stress compared to Whites and Blacks (Lorenzo-Blanco et al., 2016).
The data suggests that Hispanics are less likely to seek treatment for mental health disorders and are less likely to receive ICD-9 diagnoses in all health settings (inpatient, outpatient, emergency department, and other services). This disparity has many contributing factors. However, it is important to remember that treatment barriers come about not because of negative attitudes, but because of other structural barriers to care, including language and socioeconomic factors (Mental Health America, 2020). Prior to the passage of the Affordable Care Act, 30 percent of Hispanics lacked health insurance, versus 11 percent of non-Hispanic whites (Mental Health America, 2020). In terms of overall prevalence, psychiatric disorders are more likely among second and third-generation men and women (Alegria et al., 2007). This information suggests that mental health disorders across the Latino population in the United States are a growing concern as the protective factors of first-generation Latinos fade into second, third, and further generations. Therefore, it is important to continue to conduct qualitative and quantitative research to better define the mental health needs of the Latinx population in America. This research can then be used to develop and promote culturally competent mental health services across the United States for the Latinx population.
General Solution
To address the mental health needs of the Latinx population in Columbia, SC the following steps should be taken:
-
Qualitative and quantitative research should be done in Columbia, SC to better define needs within the Latinx population.
-
Implementation of evidence-based practices and culturally competent mental health services should be incorporated into health care systems.
-
Mental health related community health programs should be rolled out with the help of existing organizations
See how my Key Insights contribute to this solution
scroll
Multidisciplinary Thought
As discussed on the Multidisciplinary Thought page, diverse perspectives can be beneficial as they often provide complementary solutions to the same problem. For the general solutions outlined above, it will be important to include diverse perspectives from a variety of disciplines including mental health practitioners, public health practitioners, community leaders, and members of the community for which the intervention is intended to benefit. These groups can be included as stakeholders which help develop and influence the programs rolled out. Additionally, the different health beliefs and barriers to mental health care seeking in the Latino population should be considered. For this, it will be beneficial to think through the Theory of Planned Behavior for mental health care seeking (see below) as part of the planning process for these interventions and programs. This simple model is backed in the multilevel approach to health care seeking behavior that includes insight from the Socio-Ecological model also referenced on the Multidisciplinary Thought page.
Planning & Progress
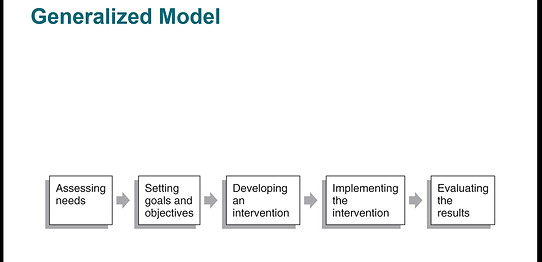
Planning adapting, and reflecting are essential for success in life and the implementation of health promotion programs. The Generalized Model (below) discussed in HPEB 300: Introduction to Health Promotion, Education, and Behavior and used in my colorectal cancer promotion project provides the perfect process outline to assure proper planning and follow-through. In line with the first step of the Generalized Model (below) and the first step in my general solution (above), a needs assessment of mental health needs and services should be completed, working with community partners such as The Good Samaritan Clinic (GSC) (which provides free healthcare services for the Latinx community), and PASOs (which means steps in Spanish and is an organization that supports the Latinx community of South Carolina through education, advocacy, and leadership development) would be excellent places to collect more information about the needs of the community. Steps 2 - 5 of the Generalized Model, should then be carried out for the general solutions suggested above. When evaluating the results a Strengths, Weaknesses, Opportunites, and Threats (SWOT) analysis discussed on the Planning & Progress page should be done. Steps for quality improvement should also be taken to adapt the programs and interventions to best fit the needs of the community.
Mitigate Misconceptions
Even though these programs and interventions should be implemented across the United States, as discussed on the Mitigate Misconceptions page, community-level interventions are most important for making the largest impact. Thus, the interventions and programs will focus on the Columbia, South Carolina Latinx community. This will allow community health educators to build relationships and trust within the community which will help the programs be successful. Additionally. the interventions and programs should be supported by research (in other words, evidence-based practice). This will promote the best outcomes, transparency, and community buy-in. In relation to Latinx mental health needs and services specifically, the first step taken to define the needs within this population with qualitative and quantitative research should help to mitigate misconceptions about mental health beliefs and care-seeking behaviors.
Goals & Objectives
Objectives and goals should be set for each step of the Generalized Model: performing needs assessment, developing the interventions, implementing the interventions, and evaluating the interventions. These should include process, learning, behavioral, and outcome objectives. Some specific goals for developing accessible community mental health programs include:
Implementation
Working with the organization PASOs, The Good Samaritan Clinic (GSC), National Alliance on Mental Illness (NAMI), and local mental health care professionals, a pilot program promoting positive mental health among the Latinx community would be initiated in the GSC. A pre-test assessing patient’s knowledge of positive mental health habits, signs of depression and anxiety and other common mental illnesses, and resources in the community and online for treatment would be given to all patients at the GSC. A class instructed by licensed community health educators would be provided Tuesdays and Thursdays to those interested and flyers with basic information on mental health care would be handed out at the clinic. There would also be one opportunity each month to seek mental health care at each of the GSC clinic locations in Columbia.
The following chart should be followed as an estimated timeline
Budget
Certain costs will be associated with this program as detailed below. To attain funds for the implementation of this, I would look to work with the GSC (Good Samaritan Clinic) to apply for service block grants from the United States Government Department of Health and Human Services, funding from the Centers for Disease Control and Prevention through groups including the Substance Abuse and Mental Health Services Administration, Mental Health America. I could also use the online service, Grant Watch, to seek further funding opportunities.

Evaluation
To evaluate the program, post-tests will assess participants’ knowledge gained from the information sessions and flyers. The pre and post-tests would be used as part of the evaluation of the program to see if it is effective in increasing knowledge. A successful session would have an average post-test score of 70% or higher as determined by standard grading scales. As this intervention will also address access to care and care-seeking behavior at the monthly psychiatric clinic, the number of patients helped will be recorded and two surveys will be given to patients. One survey will collect reasons for attending/seeking treatment and the other will collect information on previous care. A report detailing the outcomes of the intervention would be written and copies would be distributed to stakeholders and grant providers. After the pilot period, improvements would be made to the intervention as needed and continued. If proven successful in Columbia, SC, similar programs can be initiated at the other GSC’s across South Carolina.
References
Alegría, M., Mulvaney-Day, N., Torres, M., Polo, A., Cao, Z., & Canino, G. (2007). Prevalence of Psychiatric Disorders Across Latino Subgroups in the United States. American Journal of Public Health, 97(1), 68-75. doi: 10.2105/AJPH.2006.087205
Bridges A. J., Andrews A. R., & Deen T. L. (2012). Mental health needs and service utilization by Hispanic immigrants residing in mid-southern United States. Journal of Transcultural Nursing, 23(4), 359–368. doi:10.1177/1043659612451259
Delphin-Rittmon, M. E., Flanagan, E. H., Andres-Hyman, R., Ortiz, J. A., Mona, M., & Davidson, L. (2015). Racial-Ethnic differences in access, diagnosis, and outcomes in public-sector inpatient mental health treatment. Psychological Services, 12(2), 158–166. doi: 10.1037/a0038858
Kessler, R. C., Chiu, W. T., Delmer, O., & Walters, E. E. (2005). Prevalence, severity, and comorbidity of twelve-month DSM-IV Disorders in the National Comorbidity Survey Replication (NCS-R). Archives of General Psychiatry, 62(6), 617–627. doi: 10.1001/archpsyc.62.6.617
Lee S., Laiewski L., Choi S. (2014). Racial-Ethnic Variation in U.S. Mental Health Service Use Among Latino and Asian Non-U.S. Citizens. Psychiatric Services, 65(1), 68-74. doi: 10.1176/appi.ps.201200430.
Lorenzo-Blanco, E., Torres, M. E., Smithwick, J., & Wilton, A. (2016). Mental health access and the latino communities of South Carolina: An assessment of needs, existing resources, and current challenges.
World Health Organization. (2001). Mental disorders affect one in four people. Retrieved from https://www.who.int/whr/2001/media_centre/press_release/en/